When Ergoweb teaches job assessment techniques, we often start with the scientific foundation for the methods we believe to be the most useful in the identification and prevention of work-related musculoskeletal disorders (WMSDs). There are numerous assessment techniques in use, but only some of them are evidence based. We use this graphic as a way to represent the various scientific perspectives that contribute to our understanding of WMSDs:
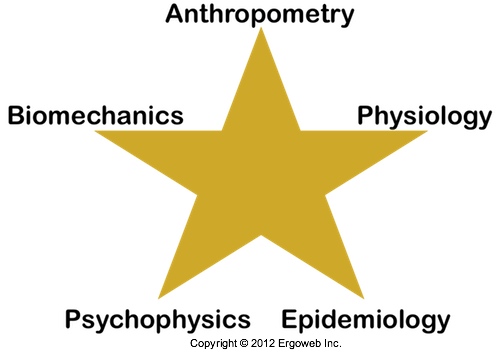
We think of this image and the scientific basis for ergonomics like a “five star base” that provides stability for an office chair. Reading the article “Job Analysis Techniques for Distal Upper Extremity Disorders,” by researchers Arun Garg and Jay M. Kapellusch, reminded me of this image, and of the importance of applying evidence based tools in ergonomics.
Garg and Kapellusch do an admirable job summarizing the state of distal upper extremity — hand/wrist/arm — analysis methods. They cover biomechanical, physiological and psychophysical analysis, the epidemiology of physical risk factors, and specific job analysis tools including:
- Rodgers Muscle Fatigue Model
- Ergonomic Job Measurement System (EJMS)
- State of Washington Industrial Safety and Health Act (WISHA) Checklist
- RULA: Rapid Upper Limb Assessment
- Threshold Limit Value (TLV) for Hand Activity Level (HAL)
- Strain Index
In this article, Part 1 of a 2 part series, I’ll provide an brief overview of their review of the applicable science, summarizing specific data regarding hand/wrist/arm characteristics and MSD risk. In Part 2, I’ll summarize their review of the specific analysis tools mentioned above, and include my own thoughts based on real-world field use of the methods. Interested readers are directed to the 47 page chapter, referenced below, for complete details.
Biomechanics: Muscle Strength
Understanding human strength capabilities and limitations is a cornerstone of the ergonomics scientific foundation. Laboratory and field experience make it clear that people can work at their maximums only infrequently, and those maximums are directly affected by factors such as posture, duration and repetition. I found the following key pieces of information from this chapter especially informative.
Regarding Grip Strength:
- pinch grip strength is roughly 80% lower than power grip strength;
- female population grip strength is about 40% lower than male population grip strength;
- there is large variation in population grip and pinch strength, influenced by:
- grip span;
- forearm rotation;
- elbow flexion and;
- wrist posture.
- optimal power grip span appears to be between 3.8 cm and 6.4 cm, influenced by gender, hand size and type of grip;
- it’s not clear what the optimum pinch grip span is, though it should not exceed 2 cm;
- 25 degrees or less of wrist extension or ulnar deviation maintains optimal grip strength;
- wrist flexion has a large effect on grip strength (more deviation = less strength);
- grip strength maximizes in forearm supination and minimizes in forearm pronation;
- grip strength is maximum at an elbow angle of 0 degrees flexion and reduces by 6% at 135 degrees flexion;
- pinch strength is lowest with wrist flexion; and
- in some situations, wrist strength may be more of a limiting factor than grip strength.
Physiology: Localized Muscle Fatigue
Although muscle fatigue, which can cause discomfort and pain, makes an intuitively appealing basis for injury mechanism (my words, not the authors’), and therefore a basis for analysis tools, its role in MSD causation remains unclear. For example, muscle fatigue is common after strenuous exercise, and strenuous exercise does not always, or even often, lead to injury (though it certainly can lead to temporary pain and discomfort, either of which can affect performance). Although persistent localized muscle fatigue and discomfort can be linked to “a diseased state,” there is a lack of evidence to generalize this to an MSD model, especially when considering that the onset of an MSD can take anywhere from hours to months after exposure.
Garg and Kapellusch pull these interesting findings from the literature:
- intermittent handgrip contractions greater than or equal to 17% MVC (maximum voluntary contraction) were unacceptable;
- continuous handgrip contractions greater than or equal to 10% MVC were unacceptable;
- one study recommends a force of 14% MVC for intermittent static contractions and 7.9% MVC for continuous static contractions; and
- muscle fatigue has been linked to decreased productivity for upper extremity tasks, particularly for arm-elevated working postures.
Psychophysics: Maximum Acceptable Workload
Psychophysics is a type of research that looks at human response to stimuli. An eye exam or a hearing test are examples, but for ergonomics, the studies generally “use a method of self-adjustment to determine maximum acceptable workload.” Examples of data collected through psychophysical studies include the well known “Snook” tables (actually a series of studies by Snook and Ciriello, or Snook at al, funded and conducted in labs at Liberty Mutual). In these types of studies, workers are generally provided with instructions to maximize their performance within constraints (e.g., “don’t get fatigued”) and given control over at least one variable, such as the amount of weight lifted, while all other task variables are controlled by the experimenters (such as the size of the box, lift distance, the pace of work, etc.).
In essence, in my words, not the researchers, the theory behind psychophysical studies in ergonomics is that given the choice and proper instructions/training, people will develop working habits that will maximize performance while preserving health and safety; or at least they will in a “perfect world.” In the absence of perfection, there are some limitations in the psychophysical scientific base, including these noted by Garg and Kapellusch:
- experimental participants are often given instructions to imagine that they will perform a given task for some period of time, like an 8 hr day, yet the experiment does not actually replicate a full 8 hr day, and may be less than 1 hr;
- there is concern that these limitations do not accurately reflect working maximums for jobs that occur 8 hrs a day, day after day, and they cite evidence that “maximum acceptable torque for 5 days per week of exposure was 36.3% lower than that for 2 days per week of exposure”;
Even with such limitations in mind, there is a significant body of research that overcomes, at least in part, these limitations and draws applicable conclusions (the Liberty Mutual studies, for example, were quite extensive and occurred over many years). Examples they include:
-
maximum acceptable frequency in a drilling task decreased by 12% with wrist flexion of 25%, and decreased by 27% at 50 degrees of wrist flexion;
-
studies that asked workers to rate discomfort, perceived exertion, fatigue or pain found:
-
a tool weighing between 0.9 Kg and 1.75 Kg (2.0 lb. and 3.9 lb.) was “just right”;
- required grip force for tools weighing less than or equal to 2 Kg (4.4 lb.) was “very comfortable”;
- a tool handle diameter less than or equal to 3.8 cm (1.5 in.) was “just right”;
- the most comfortable working height with a tool was between 102 cm and 153 cm (40.2 in. and 60.2 in.);
- the most comfortable horizontal working distance for tool use was within 38 cm (15.0 in.) of the worker; and
- repetitive work should be conducted near elbow height.
-
Epidemiology: Risk Factors
Epidemiology research looks for correlations or associations between physical factors and incidence of MSDs, and are used to provide a basis for job analysis techniques in and of themselves, or as a means to validate analysis methods. These studies require clear definitions of, and the means to measure, specific risk factors as well as specific MSD case definitions. Unfortunately, there is a lack of consistency among these important measures in the scientific literature. For example, approaches to quantifying physical exposures have included:
-
self-reported questionnaires;
-
job title classifications;
-
straightforward observations;
-
professional opinions; and
-
measurements from video, force gauges, EMG, and electrogoniometry.
Further, MSD case definition methodologies have included:
-
self-reporting by the study participants;
-
examinations by a qualified health professional; and
-
“physical examination plus related maneuvers and/or tests, such as nerve conduction studies for nerve-related disorders.”
That is, there is no standard measurement methodology, which makes it difficult to combine and generalize research findings. Garg and Kapellusch nevertheless conclude that, “However, when evaluated as a whole, despite these inconsistencies, the literature shows substantial evidence of association between job physical demands and [hand/wrist/arm] MSDs.”
The authors go on to note that even though it is not the most prevalent MSD, Carpal Tunnel Syndrome is the most commonly studied MSD. Regardless, in general, the risk factors for hand/wrist/arm MSDs are understood to include:
- forceful exertions;
- awkward hand/wrist postures;
- high repetition; and
- exposure to hand or arm vibration exposures.
As Garg and Kapellusch state, “What is not clear is how to define ‘high force,’ ‘high repetition,’ and ‘awkward posture’ and precisely what effect they have on rate of DUE [Distal Upper Extremity] MSDs, because different studies have used different measures and different values for high force, high repetition, and awkward posture.” They reference a variety of studies that have shown associations between MSDs, high forces, awkward postures, high repetitions, or combinations of such factors. They also reference studies that have proposed additional risk factors, including “unaccustomed work; stress concentration; hand, wrist, or forearm contact with sharp surfaces; duration of task per day; insufficient recovery time; static work; pinch grasp; exposure to cold temperature; and poorly fitting gloves,” and even job rotation, but they don’t believe there is enough evidence to “draw firm conclusions.”
I am somewhat surprised that Garg and Kapellusch do not include duration of exposure as a key risk factor, because my own review of the recent scientific literature suggests it is. See, for example, Force? Repetition? Posture? Duration? Which Risk Factors are Most Important in MSDs?.
In the next installment of this 2 part series, I’ll summarize their review of the efficacy of specific job analysis techniques, including Rodgers Muscle Fatigue Model, Ergonomic Job Measurement System (EJMS), State of Washington Industrial Safety and Health Act (WISHA) Checklist, RULA: Rapid Upper Limb Assessment, Threshold Limit Value (TLV) for Hand Activity Level (HAL), and the Strain Index.
Reference
Arun Garg and Jay M. Kapellusch, (2011), Job Analysis Techniques for Distal Upper Extremity Disorders, appearing in Reviews of Human Factors and Ergonomics, 7:149, DOI: 10.1177/1557234X11410386. At the time of this writing, this chapter was available online to Reviews of Human Factors and Ergonomics subscribers at: http://rev.sagepub.com/content/7/1/149
This article is reprinted, with permission, from The Ergonomics Report Archives, where it originally appeared on September 5, 2012.
